Realistic medicine is a useful concept describing healthcare that puts patients at the centre of decision making and treatment, with an aim to reduce harm, waste and unwarranted variation. One of the great challenges in medicine today is supporting patients with incurable disease in their treatment choices. Advising patients on interventions that offer reducing benefits in the face of increasing potential harms, when they may feel obliged to “take all treatments going”, requires honesty, candour and data. Realism is a better term than futility, but they are two sides of the same coin.
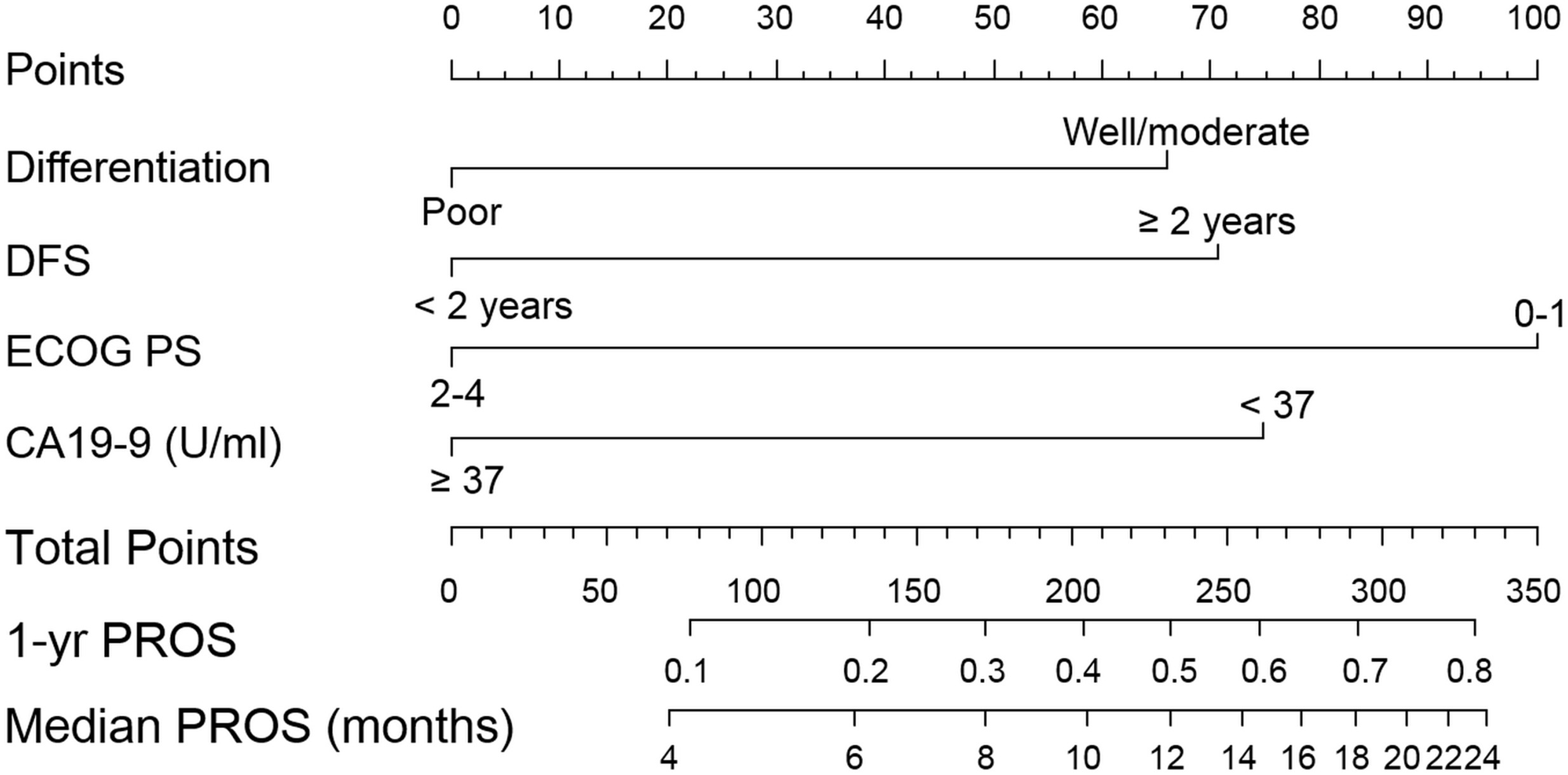
In HPB, Kim and colleagues examine survival after recurrence of bile duct cancer. The facts of this disease are always sobering: the median survival after diagnosis of recurrence is 7 months. The study is useful in that the authors have sufficient numbers to examine subgroups of those with recurrence to identify which patients may potentially benefit from salvage treatment (which was mostly chemotherapy). For those with poorly differentiated primary tumours, a short time to recurrence, poor performance status and elevated CA19-9, survival was only a handful of months.
This is a pragmatic non-randomised study with inherent selection bias, but the aim was not to determine the potential benefit of salvage treatment (we await the full publication of studies such as BILCAP). Also, the predictive ability of the model was not particularly high (c-statistic= 0.65). However, it does serve to illustrate the important point that for some very unfortunate patients with poor-prognosis recurrence, survival will be short and they may be better advised to focus on priorities other than chemotherapy. As Atul Gawande remarks in Being Mortal, “We’ve been wrong about what our job is in medicine. We think our job is to ensure health and survival. But really it is larger than that. It is to enable well-being.”